Clinical Basis
As one of the four-parts in the Transitions of Care measure, medication reconciliation is a critical part of post-discharge care coordination for all patients taking prescription medications. Patients who have more than one chronic condition are likely to take more medications; therefore, ensuring proper medication reconciliation is imperative to preventing unintended complications.1
It is a best practice to conduct the medication reconciliation within seven days of discharge.
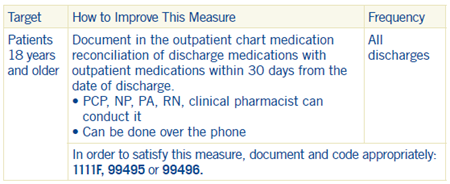
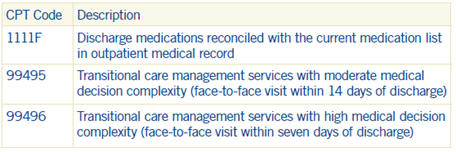
Coding and Documentation Guidance
Hospital Best Practices
Promptly send PCP a discharge summary containing a list of discharge medications. The Joint Commission identifies five steps in the medication reconciliation process:
- Obtain a list of out-patient medications.
- Obtain the list of medications prescribed at discharge.
- Compare the medications on the two lists.
- Make clinical decisions based on the comparison.
- Communicate the new list to appropriate caregivers and to patients.
Group Best Practices
Prior to discharge, schedule a PCP appointment with patients within seven days:
- This is the best time to do medication reconciliation.
- The reconciliation may be conducted by a PCP, NP, PA, RN or clinical pharmacist and may be done telephonically.
PCP Best Practices
- Document the reconciliation in the outpatient medical record with an appropriate chief complaint, such as “post-discharge hospital follow-up.”
- Include a dated progress note stating “Hospital (or skilled-nursing facility) discharge medications were reconciled with the current outpatient medications.”
1 National Quality Measures Clearinghouse (NQMC). Rockville (MD): Agency for Healthcare Research and Quality (AHRQ); 2015 Oct 01. [cited 2016 Nov 15] Go to https://qualityindicators.ahrq.gov/ for additional information.